Introduction to the research topic
Skin tumors are one of the most common types of cancer in Germany. Repeated exposure to harmful environments, especially getting sunburnt too often, leads to healthy skin cells transforming into cancerous cells. The processes in these cells have been mostly solved over the past few decades with the help of modern molecular-genetic methods of investigation. This knowledge allows the development of therapies targeting tumor cell development and propagation. These immunotherapies are especially promising against skin tumors, in particular the quickly spreading black skin cancer (melanoma). With custom-made medications, so called „immune checkpoint inhibitors“, the medication can interfere with the control processes of the cellular immune response and reactivate the body’s recognition and destruction of cancer cells. These modern immunotherapies give hope for tumor regression to patients with advanced, metastasized diseases.
Reactivation of the body’s immune response against cancer cells
„Immune checkpoint inhibitors“ custom-made at the molecular level activate the T lymphocytes of the body’s defense system. They use the lock-and-key model to identify foreign and defectively formed molecules on the cell surface (antigens). Modern immunotherapy targeting cancer reactivates T lymphocytes against cancer cells. This removes the camouflage from the immune system’s invisible enemy. This treatment method was originally developed for patients with melanoma and was subsequently used for other types of cancer (for instance lung tumors) with noteworthy success.
Investigation of the causes of therapeutic setbacks
Despite the noticeable progress in therapy, many tumor diseases are deadly. Even targeted immunotherapy often only has a temporary effect. It is also not uncommon for immunotherapy to have no effect on advanced cases. The reasons for the failure of therapy are being investigated by many research groups worldwide. One of these groups is an international team of researchers lead by Prof. Dr. Thomas Tüting, Director of the Department of Dermatology in Magdeburg and project leader of SFB 854 project A27.
A good neurotransmitter switches sides
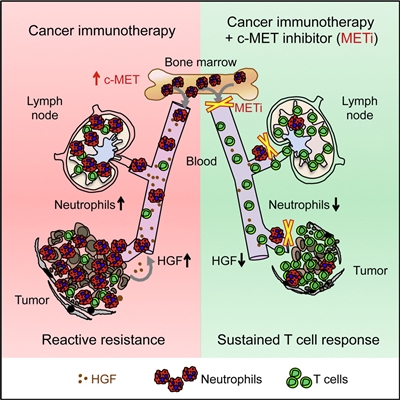
In order to understand the limits of modern immnotherapy, the researchers developed an experimental model using mice. „We realized that immunotherapy does not only activate the T lymphocytes against cancer, but also the immune cells in the bone marrow, the so called polymorphonuclear neutrophils“, said Professor Tüting. Polymorphonuclear neutrophils defend against bacterial infections and can also attack cancerous cells. In the latter case, these attacks can be blocked by the use of various molecular camouflage techniques. „In this case, the cancerous tissue can act like normal, injured tissue and triggers an inflammatory reaction“, explained external lecturer Dr. Gaffal, Senior Physician at the Department of Dermatology in Magdeburg and coauthor of the study. This is made possible by a hepatocyte growth factor, which the polymorphonuclear neutrophils produce. „The body’s chemical signals prevent the T lymphocytes from fighting cancerous cells instead of helping“, explained the first authors of the study, Nicole Glodde and Tobias Bald, when describing the study results with genetically modified mouse stem cells. „It is as if this signal brings out a second personality in the immune cells, similar to the famous case of Dr. Jekyll, who transforms into the merciless killer Dr. Hyde when he drinks a mysterious potion“, described Prof. Dr. Michael Hölzel from the Institute of Clinical Chemistry and Clinical Pharmacology in Bonn.
On the path to improving immunotherapies targeting cancer
Through the targeted inhibition of the released growth factor, the research group was able to significantly increase the effect of the immunotherapy in an experimental animal model. „The next step is to initiate clinical studies in order to see how these discoveries can be used in normal practice on cancer patients“, said Prof. Tüting. „The established research groups at Magdeburg’s university including the Collaborative Research Center 854 and the Health Campus: Immunology, Infectiology and Inflammation (GC-I³) offer excellent conditions for these ambitious goals.“
Text: Uwe Seidenfaden
Publication: Reactive neutrophil responses dependent on the receptor tyrosine kinase c-MET limit cancer immunotherapy. Immunity, 2017 Oct 17;47(4):789-802.
Picture: Graphical Abstract (Source: original publication)
Researchers from Magdeburg and Bonn have new insights regarding the effectiveness of immunotherapies targeting cancer
An international team led by researchers from the university hospitals in Magdeburg and Bonn discovered a braking mechanism initiated by the body, which has limited the effectiveness of immunotherapies targeting cancer until now. Furthermore, the scientists were able to show that a combination of targeted inhibitors turn off this mechanism and can improve these immunotherapies. The results of their research were published in the current issue of the prestigious journal „Immunity“.